Breast cancer and diabetes appear to be two distinct diseases, with the only thing they have in common is how common they are. Breast cancer is the second most commonly diagnosed malignancy after certain types of skin cancer; one in every eight American women will develop invasive breast cancer at some point in their lives. The most common type of cancer among women is breast cancer. More over, 10% of Americans have diabetes, and it is expected that 20% of the population will develop the chronic disease at some time in their lives.
Previous studies, on the other hand, have discovered a link between the two disorders. Diabetes, for example, raises the risk of breast cancer in women by 20% to 27%. Insulin resistance, a hallmark of diabetes, has been linked to a higher risk of breast cancer and a reduced likelihood of survival.
A population-based study found that two years after a breast cancer diagnosis, the chance of developing diabetes increases. Breast cancer survivors are 20% more likely than age-matched women who do not have the disease to develop it ten years following diagnosis.
However, these epidemiological connections aren’t always clear, and some studies have found no association between the two.
A study team led by researchers from the University of California San Diego School of Medicine discusses a proposed genetic mechanism linking the two diseases in a new publication published in Nature Cell Biology on May 30, 2022.
Breast cancer reduces insulin synthesis, leading in diabetes; on the other hand, poor blood sugar control increases tumour growth, according to this mechanism.
Shizhen Emily Wang, PhD, professor of pathology at the University of California, San Diego School of Medicine and research co-author, added thar no illness is an island, just as no cell survives alone. The study shows how breast cancer cells influence pancreatic islet function. As a result, they produce less insulin than is needed, resulting in higher blood glucose levels in breast cancer patients than in cancer-free women.
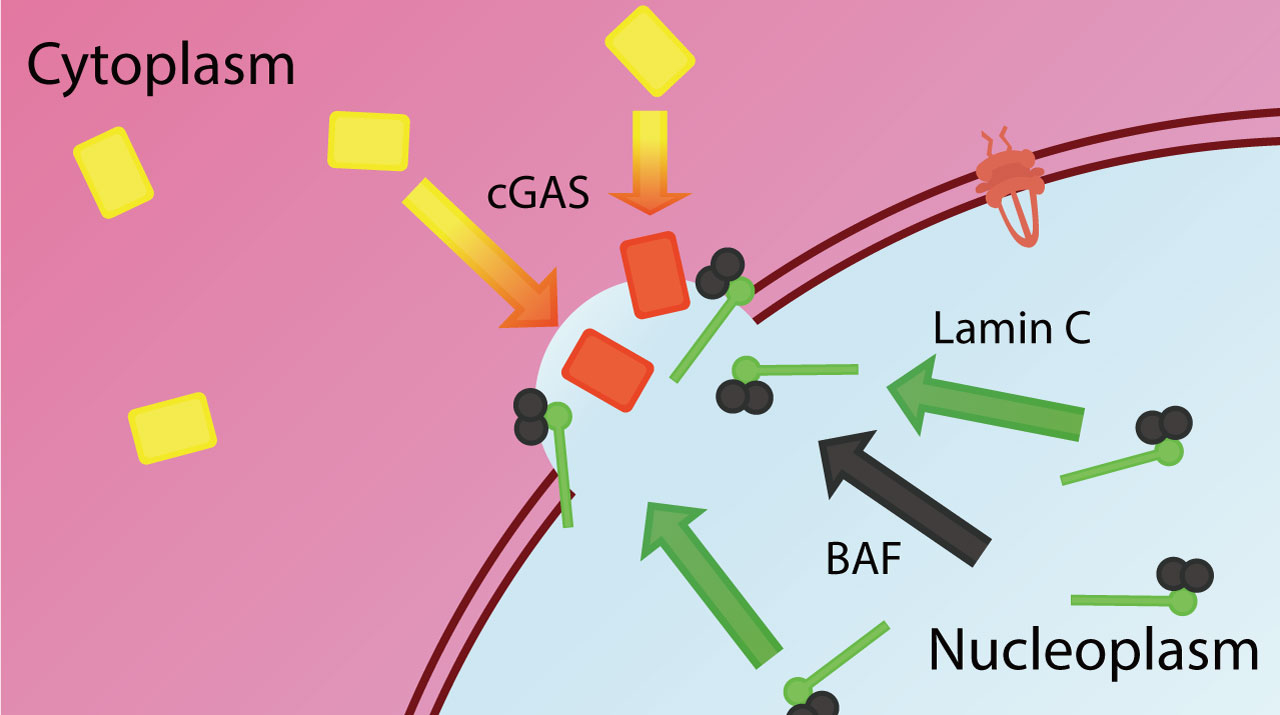
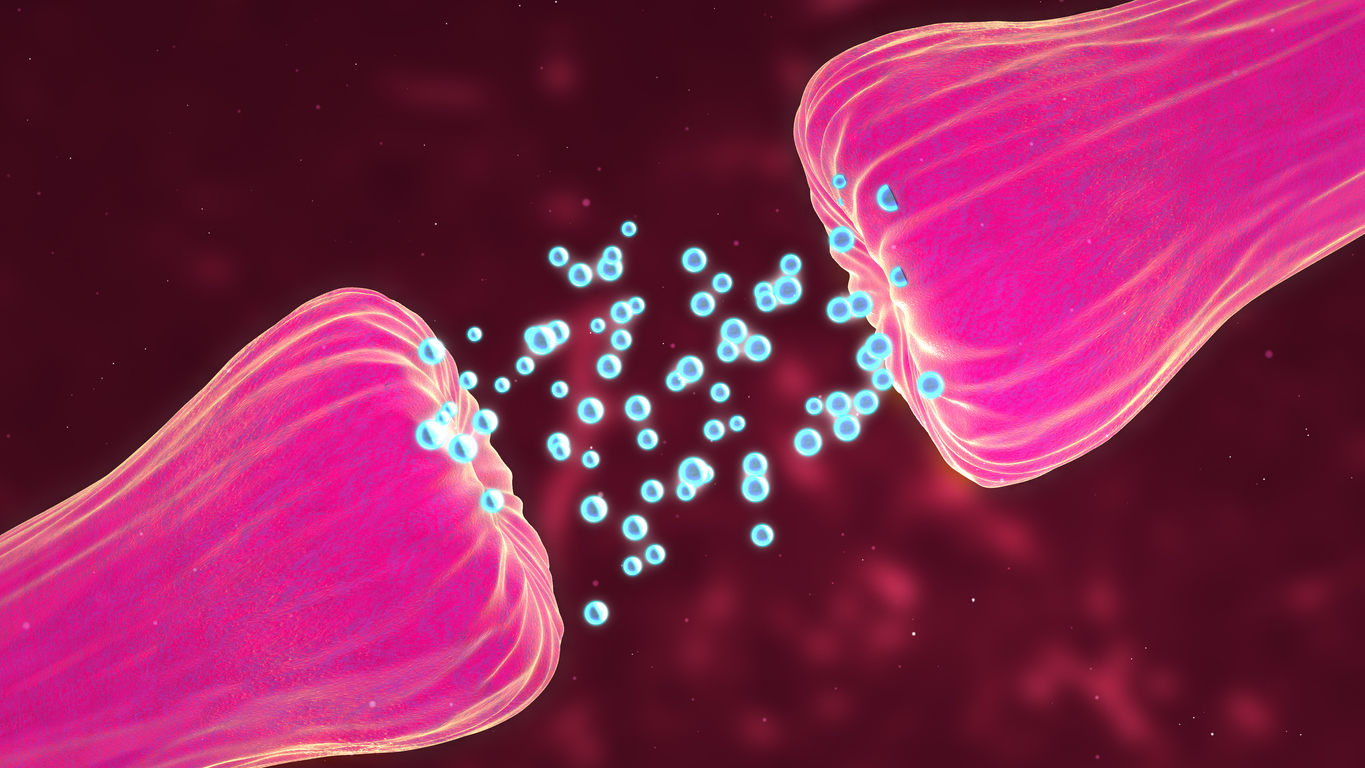
Extracellular vesicles (EV) are hollow spheres that are released or shed by cells and operate as a cargo communication system by transporting DNA, RNA, proteins, and lipids between cells.
Cancer cells released microRNA-122 into the vesicles. According to Wang, once vesicles reach the pancreas, they can infiltrate insulin-producing islet cells, release their miR-122 payload, and impair the islets’ critical role in blood glucose management.
To fuel tumour growth, malignant cells use more glucose than healthy cells. The use of PET scans in cancer diagnosis is based on this finding. Breast tumours offer cancer cells with their preferred fuel source by increasing the amount of glucose in the blood, which cancer cells can consume right away. Healthy cells, on the other hand, are deprived of this vital component.
Researchers used mouse models to show that slow-release insulin pellets or an SGLT2 inhibitor, a glucose-lowering medicine, can restore normal glucose control while suppressing tumour growth in the presence of a breast tumour.
These findings support a greater need for diabetes screening and prevention among breast cancer patients and survivors, according to Wang, noting that a miR-122 inhibitor developed by San Diego-based Regulus Therapeutics Inc. is currently being tested in clinical trials as a possible treatment for chronic hepatitis C.
These findings show that breast cancer patients and survivors have a greater need for diabetes monitoring and prevention. In breast cancer mice models, it has been demonstrated to aid in the restoration of normal insulin production and the prevention of tumour formation.
The miR-122 inhibitors, which are the first miRNA-based medications to enter clinical trials, may have a new application in the treatment of breast cancer.
Story Source: Original press release by University of California – San Diego.. Note: Content may be edited for style and length by Scible News.
References
Minghui Cao, Roi Isaac, Wei Yan, Xianhui Ruan, Li Jiang, Yuhao Wan, Jessica Wang, Emily Wang, Christine Caron, Steven Neben, Denis Drygin, Donald P. Pizzo, Xiwei Wu, Xuxiang Liu, Andrew R. Chin, Miranda Y. Fong, Ziting Gao, Kaizhu Guo, Oluwole Fadare, Richard B. Schwab, Yuan Yuan, Susan E. Yost, Joanne Mortimer, Wenwan Zhong, Wei Ying, Jack D. Bui, Dorothy D. Sears, Jerrold M. Olefsky, Shizhen Emily Wang. Cancer-cell-secreted extracellular vesicles suppress insulin secretion through miR-122 to impair systemic glucose homeostasis and contribute to tumour growth. Nature Cell Biology, 2022; DOI: 10.1038/s41556-022-00919-7