One of the most annoying aspects of urinary tract infections (UTIs) is their recurrence. Urinary tract infections are thought to be caused by bacteria in the urinary system and are characterised by painful and frequent urination. The majority of women who take antibiotics see an improvement in their symptoms. However, healing is usually only temporary, since one-quarter of women will get another UTI within six months. Some people are forced to take medications on a monthly basis to treat these recurrent urinary tract infections (UTIs).
Multiple urinary tract infections (UTIs) in women may be the consequence of a vicious cycle in which the medications used to treat one illness predispose them to contracting another, according to new research. Doctors from Washington University School of Medicine in St. Louis, the Broad Institute of MIT and Harvard University, and the Broad Institute of MIT and Harvard University discovered that antibiotics can kill disease-causing bacteria in the bladder but not the intestines. A second urinary tract infection can be caused by germs that stay in the stomach and invade the bladder (UTI).
Prolonged antibiotic cycles can harm the gut microbiome, a community of beneficial bacteria that lives in the intestines, in addition to causing gastrointestinal discomfort. Women with recurrent UTIs had microbiomes that were less diverse and missing a key type of bacteria that helps regulate inflammation, similar to other disorders in which gut microbes and the immune system are related. Furthermore, their blood had an immunological profile that indicated inflammation, which was similar to that of other disorders impacting gut bacteria and the immune system.
The study’s findings were published in Nature Microbiology on May 2.
It’s difficult for women who visit their doctor with recurrence after recurrence, and the doctor, who is often male, gives them hygiene advice, according to co-author Scott J. Hultgren, PhD, the Helen L. Stoever Professor of Molecular Microbiology at Washington University. However, hygeine isn’t always the source of the problem. This is usually not due to a lack of personal cleanliness. The relationship between the gastrointestinal tract and the urine bladder, as well as the levels of inflammation in the systemic circulation, are both problematic within the condition. Doctors are baffled when it comes to treating recurrent UTIs. Because antibiotics are their sole option, they treat the problem with even more medications, exacerbating the problem.
Current Study
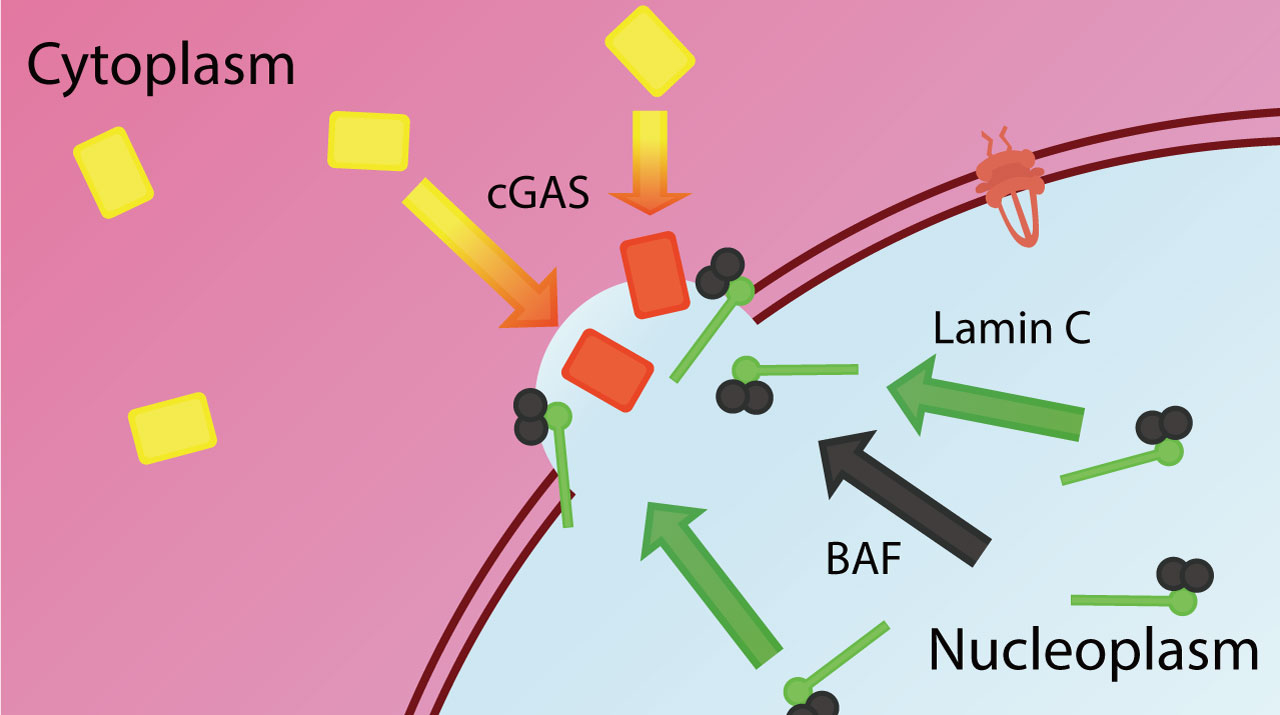
The bacteria Escherichia coli (E. coli) causes the majority of urinary tract infections (UTIs), which enter the urinary tract from the intestines. Colin Worby, PhD, a computational biologist at Broad and the paper’s principal author, collaborated with Ashlee Earl, PhD, senior group leader for Broad’s Bacterial Genomics Group, to figure out why some women get sick after getting a virus while others don’t.
The researchers looked at 15 women with a history of recurrent UTIs and 16 women who had never had a recurrent UTI. All participants provided urine, blood, and monthly stool samples, as well as other information, when the study began. The researchers looked at the bacteria in stool samples, the presence of bacteria in urine and blood samples, and the gene expression in the samples.
Every single one of the 24 recurrent UTIs that occurred over the course of a year was in a patient who had previously been diagnosed with recurrent UTI. Patients with urinary tract infections had additional urine, blood, and stool samples obtained (UTI).
Findings.
Surprisingly, the difference between women who had repeated UTIs and those who did not was determined by the kind of E. coli in their intestines as well as the presence of E. coli in their bladders. Both groups harboured E. coli strains capable of causing urinary tract infections in their intestines, and these germs were infrequently able to migrate to their bladders.
The most notable difference between the two was shown by the composition of their gut microbiomes. Patients who had several infections had a smaller range of beneficial gut microbial species, which could help disease-causing bacteria establish and spread. According to the study, bacteria that produce butyrate, a fatty acid with anti-inflammatory properties, were lacking from the microbiomes of women with recurrent UTIs.
Conclusions
The findings underscore the importance of looking into antibiotic alternatives for treating urinary tract infections (UTIs).
Antibiotics, according to Worby, may not prevent repeated infections or eliminate UTI-causing bacteria from the stomach, but instead may increase the risk of recurrence by maintaining a disturbed microbiome.
Hultgren has spent a lot of time trying to come up with new ways to get disease-causing E. coli strains out of the body while keeping the rest of the bacterial community safe. His findings paved the way for sugar mannoside-based medication and an investigative vaccination, both of which are now being studied on humans. Another alternative is to rebalance the microbiome through faecal transplants, probiotic foods, or any other method.
This is one of the most common diseases in the United States, if not the entire world, according to Hultgren. Furthermore, a considerable percentage of these people have recurring episodes, which significantly lowers their quality of life. It is critical to discover more effective treatments that can stop the cycle.
Story Source: Original story written by Washington University School of Medicine. Note: Content may be edited for style and length by Scible News.
Reference
Colin J. Worby, Henry L. Schreiber, Timothy J. Straub, Lucas R. van Dijk, Ryan A. Bronson, Benjamin S. Olson, Jerome S. Pinkner, Chloe L. P. Obernuefemann, Vanessa L. Muñoz, Alexandra E. Paharik, Philippe N. Azimzadeh, Bruce J. Walker, Christopher A. Desjardins, Wen-Chi Chou, Karla Bergeron, Sinéad B. Chapman, Aleksandra Klim, Abigail L. Manson, Thomas J. Hannan, Thomas M. Hooton, Andrew L. Kau, H. Henry Lai, Karen W. Dodson, Scott J. Hultgren, Ashlee M. Earl. Longitudinal multi-omics analyses link gut microbiome dysbiosis with recurrent urinary tract infections in women. Nature Microbiology, 2022; 7 (5): 630 DOI: 10.1038/s41564-022-01107-x