Antibiotic-resistant bacteria, viruses, and fungi, such as tetracycline and aminoglycosides, pose a substantial threat to the world population, and antimicrobial resistance (AMR) is projected to grow over the next several decades.
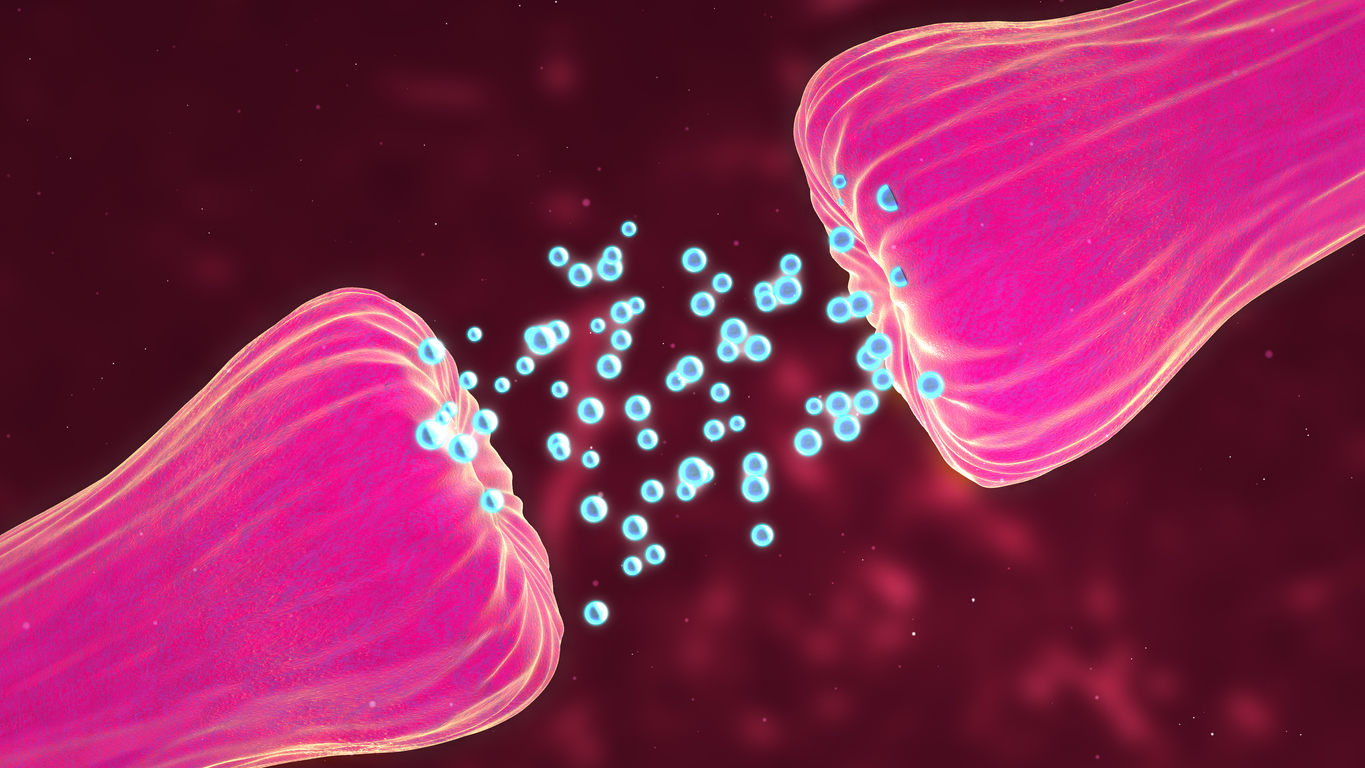
The gut microbiota is the primary cause of antibiotic resistance in humans. Gut microorganisms have genetically encoded mechanisms for surviving drug interactions, as is widely documented.
Dietary modification, according to the findings, could be a new weapon in the fight against antimicrobial resistance in the near future. This isn’t about some exotic cuisine; rather, it’s about a varied, fiber-rich diet that many Americans today are told to follow. The study was led by Danielle Lemay, a molecular biologist at the Western Human Nutrition Research Center of the Agricultural Research Service in Davis, California.
Fiber: the future weapon against antibiotic resistence?
The researchers wanted to discover if there was a link between the amount of fiber and animal protein consumed by adults and the levels of antibiotic resistance genes in human gut microbes (n= 290).
Eating a high-fiber, low-protein diet, notably from beef and pig, was consistently linked to reduced levels of antimicrobial resistance genes (ARG) in gut bacteria, according to the researchers. The people with the lowest amounts of ARG in their gut microbiomes had the most stringent anaerobic bacteria, which do not grow in the presence or absence of oxygen and are linked to a healthy gut with low inflammation.
However, it did not appear that the amount of animal protein ingested was a significant predictor of high ARG levels in the diet. According to the researchers, the most compelling evidence showed a relationship between dietary soluble fiber levels and ARG concentrations.
Nutritional diversity, rather than fiber intake, was revealed to be the most important predictor of low ARG levels in this study. This means that we should eat a variety of foods high in soluble fiber in order to gain the most benefits.
Soluble fiber is found in grains like barley and oats, legumes like beans, lentils, and peas, seeds (including chia seeds), nuts, and fruits and vegetables like carrots, berries, artichokes, broccoli, and winter squash.

The gut microbiomes of those with the highest ARG concentrations were found to be significantly less varied than those with low or moderate ARG concentrations.
Diet provides food for the bacteria that live in the intestine. All of this shows that modifying the gut microbiota through nutrition could be a long-term strategy for combating antibiotic resistance, according to Lemay.
However, because this was an observational study rather than a randomised controlled trial in which patients were assigned a specific diet, future randomised controlled trials would allow for more direct comparisons, Lemay explained.
These nutritional treatments may help to lessen the burden of antimicrobial resistance, and the findings might be used to develop dietary guidelines that look into how nutrition can help to lower the occurrence of antibiotic-resistant diseases.
Story Source: Original release written by US Department of Agriculture – Agricultural Research Service.. Note: Content may be edited for style and length by Scible News.
Reference
Andrew Oliver, Zhengyao Xue, Yirui T. Villanueva, Blythe Durbin-Johnson, Zeynep Alkan, Diana H. Taft, Jinxin Liu, Ian Korf, Kevin D. Laugero, Charles B. Stephensen, David A. Mills, Mary E. Kable, Danielle G. Lemay. Association of Diet and Antimicrobial Resistance in Healthy U.S. Adults. mBio, 2022; DOI: 10.1128/mbio.00101-22